Sleeve Gastrectomy or Vertical Sleeve Gastrectomy
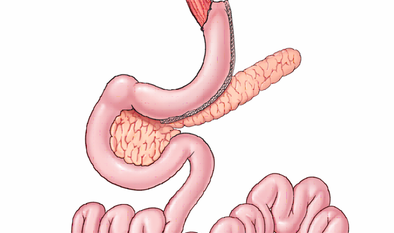
Sleeve gastrectomy or vertical sleeve gastrectomy has been around for weight loss since 2001. Sleeve gastrectomy involves removing approximately 70% of the stomach and leaving the stomach in the shape of a banana, and is usually done laparoscopically or with small incisions.
It was a procedure originally designed for people who weighed over 400 lbs and were considered too high risk to have a gastric bypass or duodenal switch because it would take a long time in the operating room to perform. So, taking out part of the stomach is a shorter operation, and the idea was that it would be safer to remove the stomach as a first stage of weight loss surgery. We hoped that the patients would lose at least 100 pounds, and then we would bring them back to surgery to bypass their intestines.
What we found was interesting!
When vertical sleeve gastrectomy patients were called to come back for the second stage of their weight loss operation, the intestinal bypass, they refused! Patients routinely lost over a hundred pounds and would not consider a second stage until their weight loss leveled off. So, that started all of us surgeons thinking, “What if sleeve gastrectomy could be a stand-alone operation for weight loss, like gastric banding and gastric bypass?”
Sleeve gastrectomy started to increase around the country slowly. Our numbers have increased significantly since we got an insurance or CPT code for sleeve gastrectomy in January 2010. Most insurance companies cover sleeve gastrectomy if weight loss surgery is a covered procedure under your plan. So why is sleeve gastrectomy the new kid on the block? We finally have five year weight loss data for the sleeve so we can measure it up against the other weight loss procedures.
The weight loss for sleeve gastrectomy is somewhere between the results for gastric banding and gastric bypass. As we do more sleeve gastrectomies around the country and the world, different hormonal aspects of the operation are becoming clearer.
Sleeve gastrectomy affects hunger because we remove the part of the stomach that makes ghrelin, a hormone that is elevated when people are hungry. We find that hunger in our sleeve patients is reduced and stays reduced long term. The operation also makes people eat a lot less because a lot of the stomach is removed.
Most of the weight loss with sleeve occurs in the first year. The follow-up with your surgeon and dietitian is crucial for ongoing success. There is another hormone, GLP 1, which is important in improving Type 2 Diabetes Mellitus. With sleeve gastrectomy, patients can expect a rise in this hormone with a resulting drop in their blood sugar and improvement or remission of their diabetes. With weight loss, Type 1 or adolescent diabetics will also see an improvement in their blood sugar and a reduction in their insulin usage.
Since sleeve gastrectomy involves the removal of a large part of the stomach, there is potential for leaks to occur. A leak is when the staple line used to make the stomach smaller is not watertight. Other procedures may be necessary to control a leak. Leak rates for sleeve gastrectomy are approximately 1%. Weight regain is also possible with the sleeve and approximately 1/15 of patients will require reoperation for inadequate weight loss or weight regain.
Find a surgeon well versed with weight loss surgery and the possible complications as well as the best treatments for weight regain if it occurs. Long-term with a sleeve, complications like bowel obstruction that can happen with gastric bypass are not common.
I encourage all weight loss surgery patients to take a multivitamin and return for the prescribed follow-up. Follow-up is approximately 5-7 visits in the first year and 2-3 in the second year. I then see patients annually. I know support groups are a great way to stay on track on your weight loss journey so definitely commit to going.